Your Cart is Empty
Free Shipping on orders $75+
Free Shipping on orders $75+
Free Shipping on orders $75+
August 05, 2022 4 min read
Not very many years ago words like “weed,” “mary jane” and “grass,” all synonyms for cannabis, weren’t voiced in polite company. Now some medical providers suggest cannabinoids, the natural chemicals found in cannabis, to treat different illnesses. But getting the medical community on board has been a rocky road.
“I have been studying the impacts of cannabinoids on the human system for over 15 years,” says Mary Brown, founder of SMJ Consulting at the Seattle-based AIMS Institute (an integrative clinic that supports all types of care under one roof, allowing MDs, naturopaths and other clinicians to collaborate). “When I began working with doctors on behalf of patients 10 years ago, they were reluctant to even engage in conversations about the potential benefits of cannabinoid therapy.”
Practitioners often remained silent because they feared repercussions from federal or state medical associations, Brown says. In many cases the medical professionals feared losing their licenses, so using cannabis was not something they publicly acknowledged, she says.
As the medical community witnessed the efficacy and heard more from the public about their interest in cannabis-based medicine, more providers became willing to have an open conversation, Brown says. Some even encouraged their patients to track their progress or lack of, as they attempted symptom management with cannabis-based medicine, so they could see the results.
A key milestone in changing the medical community’s opinion of cannabis therapy occurred when the first whole plant cannabis-based prescription medicine, trade name Epidiolex, was approved by the U.S. Food and Drug Administration in June 2018, says Dr. Sunil Aggarwal, co-founder and co-director of the AIMS Institute. In April 2020 the US Drug Enforcement Administration descheduled Epidiolex, meaning it still required a prescription but was no longer considered a controlled substance.

Brown notes she’s seeing more invitations to speak about the pharmacology of cannabinoids at global medical conferences and she believes educating practitioners will be the key to wider acceptance.
“My hope is that more providers will engage in education or at the very least accept that there is therapeutic value in many cases,” says Brown.
Patients are responding positively to the integration of cannabinoids in oncological, neurological and palliative care, but many still have questions. When his patients hesitate to try cannabinoids, Aggarwal acknowledges and validates their discomfort. He asks questions so he can better understand the basis of their preconceptions. Then he offers holistic education and counseling based on available scientific evidence and his own clinical experience so the patient can make an informed decision.
“I am also keenly aware that there may be significant barriers for patients whose jobs, conditions of their housing or court orders require drug testing,” says Aggarwal. “In these cases, I try to see what can be done from a medical advocacy or prescriptive protection standpoint.”
Because of a recommendation from the World Health Organization, the United Nations recently removed cannabis from the most restrictive controlled substance category in international law, Aggarwal says.
Brown is seeing more patients willing to enter retail stores to purchase products, but there’s a lack of medically formulated products available.
“That’s why we’ve partnered with cannabis companies and provided them with formulations that are proving effective on a large patient base both in and outside of our clinic,” says Brown. These partnerships include product development, such as with Polite, a line of high-CBD, low-THC cannabinoid wellness products, as well as partnerships with retail shops like the Bakeréé, a cannabis retail store where the staff focuses on the gaps in consumer access by providing both education and quality products, Brown says.
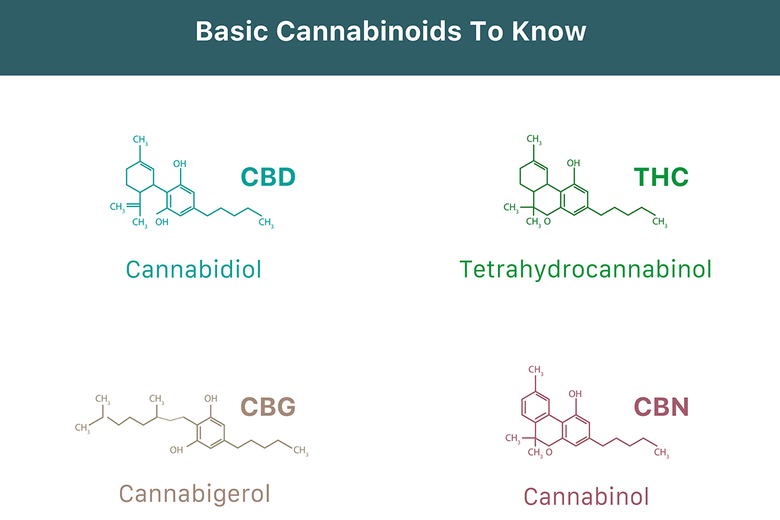
Many companies create wellness products with good intentions, but few employ physicians who formulate the final products based on observational data collected in a clinical setting, Brown says. But this is changing. Brown cites the Polite team’s deep clinical expertise in cannabinoid science and the actual practical applications and outcomes of cannabinoid therapy as critical to the development of formulations with very intentional ratios of beneficial cannabinoids beyond just CBD and THC, to include emergent nonintoxicating cannabinoids like CBG and CBN that have been researched for decades but are just now becoming more accessible.
This synergy between the medical and scientific study of cannabinoid pharmacology and the development of reliable, accessible products opens the doors for both current customers and those new to cannabis to find what they need.
Fine cannabis shouldn’t be an exclusive club. The Bakeréé acquisition team’s mission is to find the best products at every price point. We only work with suppliers that exercise responsible, sustainable practices. Our budtenders are ready to answer customer questions.
DISCLAIMER: This product has intoxicating effects and may be habit-forming. Marijuana can impair concentration, coordination, and judgement. Do not operate a vehicle or machinery under the influence of this drug. There may be health risks associated with consumption of this product. For use by adults 21 and older. Keep out of reach of children.
Comments will be approved before showing up.